We will bring a more structured and data driven approach to quality improvement and share insights to support continuous improvement across the primary health care system. We will advocate for quality and value-based primary health care that continually adapts to meet the health care needs of Western Australians, keeps people healthy, prevents disease and reduces demand for hospital services.
A new direction for general practice National data storage and analytics platform Health Professionals Networks COVID-19 Vaccine Rollout Managing pain and addiction Responding to bushfires and a lockdown Digital health making inroads Sustainable GP workforce for Kalgoorlie Upskilling GPs in urgent care

A new direction for general practice support and development
In response to the changing national primary care landscape, we have reshaped and improved the way we support general practice. These changes will allow us to offer a more tailored approach, to ensure practices receive the level of support they need, including the ability to take part in collaborative communities of practice.
Going forward, we will have a strong emphasis on helping practices to perform at the highest level, while providing patient-centred care. We will help practices to achieve this through quality improvement initiatives and the use of data to make informed decisions about primary health care delivery for their patients.
This year, we have diverted our resources to support general practice and the Australian Government Department of Health through COVID-19 outbreaks and the roll out of the national vaccination program.
We have invested in the development and ongoing maintenance of 18 localised COVID-19 HealthPathways including practice management, assessment and management, last days of life, mental health and vaccination pathways. These pathways have supported GPs to manage complex and changing advice as COVID-19 evidence has emerged.
Our support teams have provided regular and timely advice to general practice around changes to the COVID-19 vaccine program, delivered webinars, education events and regular newsletter updates.
We have advocated for general practice locally and nationally and remain committed to meeting the needs of general practitioners and the primary care community we serve.
National data storage and analytics platform:

By March 2021 the development of the Primary Health Insights data storage and analytics platform was complete and all 27 participating PHNs onboarded.
Led by WAPHA, this has been the largest and most complex national project undertaken by PHNs, and the first at this scale by PHNs operating as a collective.
Primary Health Insights is highly secure environment that stores de-identified patient data for PHNs in their individually secured ‘lock boxes’. Data is managed under the rigorous National Data Governance Framework developed by PHNs, which ensures compliance with Australian Privacy Principles and legislation.
In the near future, PHN analysts will be able to commence using the platform’s advanced analytics and reporting tools to generate new insights into population health and improve the informational support provided to primary health care providers.
“Primary Health Insights will give PHNs the capability to better understand population health, target commissioned services in areas of greatest need and support primary care services in their service provision and planning, ultimately driving better health outcomes across the country.” – Chief Digital Transformation Officer, Giles Nunis
Health Professionals Networks
We partnered with Rural Health West and Rural Clinical School and other likeminded agencies to continue to expand the Country WA regional Health Professionals Networks, with launches in the Pilbara, Midwest-Gascoyne, Wheatbelt, Great Southern and Kimberley.
Adding to the Goldfields and South West Networks launched the previous financial year, more than 1,200 health professionals are now members, with about 800 participating in Facebook groups.
Networking and education events held included sundowners; educational breakfasts and dinners; Pilbara Young Professionals Summit on Mackerel Islands and education sessions such as Palliative approach to Care for Aboriginal Health Care Professionals, Rheumatic Heart Disease, Cancer and Diabetes.
These collegiate groups provide rural and remote health professionals with better support and greater opportunities to network, upskill, share information and collaborate in their local community to support the provision of better and more joined up care and to reduce professional and social isolation experienced by rural and remote workers.

A key contributor to the COVID-19 Vaccine Rollout
This year, WA Primary Health Alliance played a key role in the COVID-19 vaccine rollout, leading the primary health care response in WA. This included onboarding 77 per cent of WA’s general practices to take part in the rollout, supporting them with clinical HealthPathways, and answering queries via our Practice Assist service.
Additionally, we worked intensively with residential aged care providers’ residents and staff, and at-risk groups, to ensure they had access to the vaccine program.
Multidisciplinary approach to managing pain and addiction
More than 60 GPs and other health professionals attended our Managing Pain – A Team Approach education event.
This combined learnings from the Persistent Pain Program and the Treating Alcohol and Drugs in Primary Care Program (TADPole) we fund in conjunction with Edith Cowan University.
Participants heard from an international pain specialist, addiction specialist and allied health professionals, and participated in interactive sessions.
The link was made via opioid use/misuse in the treatment of pain and the alternatives available in a multidisciplinary approach to managing chronic pain.
The TADPole program is funded by WAPHA with the primary aim of increasing the capacity of the WA primary care workforce to provide alcohol and drug treatment and support.
“It was a wonderful learning opportunity, so great to collaborate and learn from each other in person. All the speakers were outstanding. The whole theme of the day promoting multidisciplinary collaboration was excellently highlighted in the afternoon group sessions.” – Workshop participant

Responding to bushfires and a lockdown in one week
In a busy week in February that saw areas of Western Australia go back into lockdown, as well as devastating bushfires to the north east of Perth, WAPHA was well placed to continue supporting primary care.
We were one of the first organisations in WA to move to remote working, setting up a plan ahead team and an emergency response team, allowing the organisation to ensure its road map was in step with the uncertain environment created by COVID-19.
“This allowed us to continue to support primary care, service providers and other stakeholders without interruption, particularly given a significant amount of our interaction has been virtual since the pandemic began.” – CEO Learne Durrington
Our practice support team remained in regular communication with general practices to help keep them, their staff and their patients safe and more than 200 funded service providers were supported remotely via local teams with information and resources.
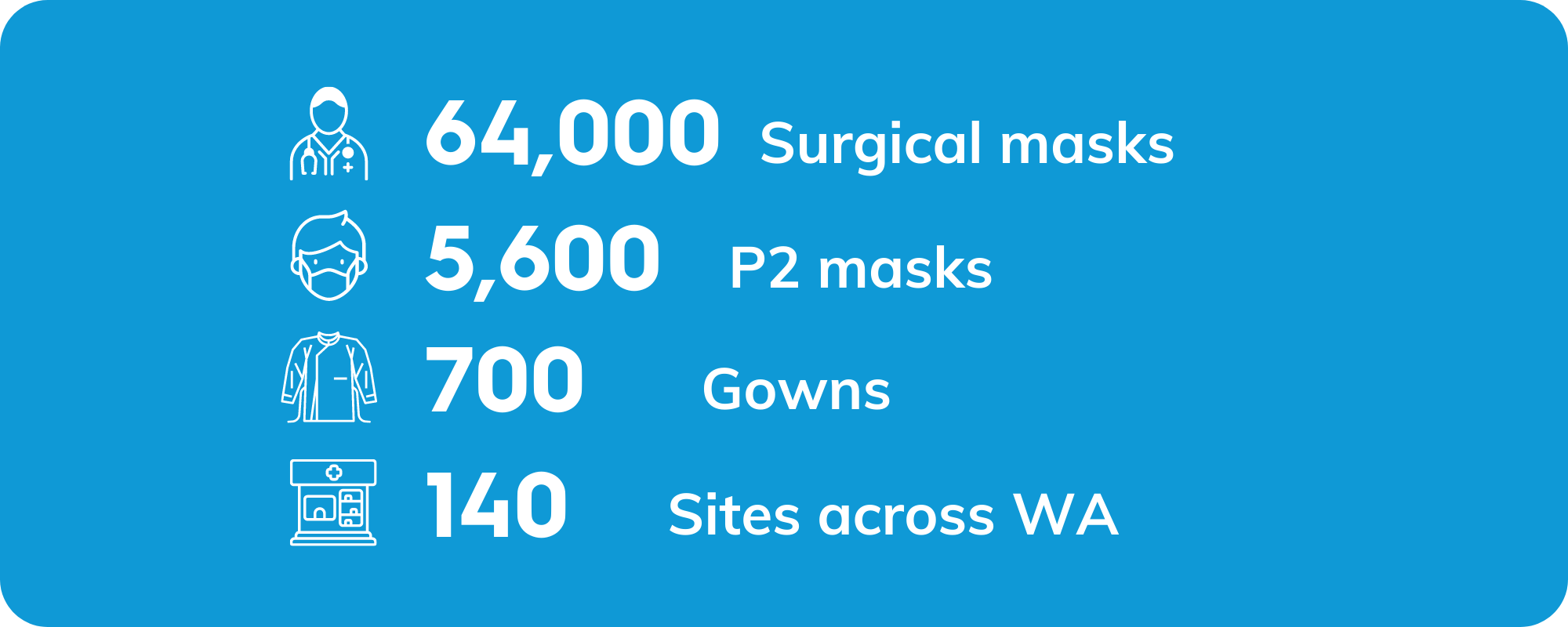
An unprecedented demand for personal protective equipment was met, with WAPHA’s logistics team overseeing the dispatch of:

Digital health making inroads
Our Digital Health Team has been busy both virtually and, on the road, supporting clinicians and communities to adopt and use digital health tools.
The significant boost in digital health usage by clinicians continued to build following the initial flurry of uptake in telehealth consultations and electronic prescribing in the early stages of the COVID-19 pandemic.
This year, views and uploads to My Health Record increased. In June 2021, shared Health Summary and Dispense Record uploads hit 610,903 and views rose from 116,213 to 219, 046 in June 2021, indicating the increased value being found by clinicians.
The option to provide electronic scripts was made available to general practices at the start of the year, leading to 414,068 eScripts being dispensed from 1,196 prescribers by June.
Mapping solutions to a sustainable GP workforce for Kalgoorlie
Leveraging the strengths of our strong stakeholder relationships in Kalgoorlie, an exciting opportunity presented to work together to build a sustainable GP workforce for the Kalgoorlie community.
WAPHA partnered with Rural Health West, WA Country Health Service, WA GP Education and Training, the Rural Clinical School and researchers from Curtin University to undertake a Naïve Inquiry to map out solutions to the GP workforce shortage and a more sustainable future.
The purpose of the initial survey and subsequent interviews was to seek perspectives on the reasons for the current GP workforce attraction and retention issues in Kalgoorlie.
Findings from interviews undertaken with GPs in the Goldfields were shared with stakeholders to inform a follow up forum where stakeholders considered options for addressing the professional and lifestyle challenges reported through the Inquiry interviews.
A Deliberative Forum was held with GPs and other stakeholders in Kalgoorlie focused on mapping future pathways.
Two key outcomes included collective advocacy to seek change to Kalgoorlie’s Modified Monash Model status and investigating changes required to existing clinical models in the region that are needed to attract and retain safe, quality and full scope of practice Rural Generalist GPs.


Upskilling GPs in urgent care
As part of the GP Urgent Care Network Pilot, this year 114 participating GPs from the Perth Metropolitan and South West regions benefitted from intensive education sessions facilitated by the Royal Australian College of General Practitioners (WA Branch) on topics including mental health, abdominal health and hand injuries.
Sixteen well attended courses for clinical general practice staff were run across Perth and the south west, either by the University of Western Australia’s Clinical Training & Evaluation Centre or the Benchmarque Group Registered Training Organisation.
A joint initiative of the Department of Health WA and WAPHA, the Pilot uses existing capacity and capability within general practice to provide care for patients with urgent but non–life-threatening medical conditions, as a minimal cost solution, with a view to developing a sustainable GP-led urgent care model into the future.
Future considerations for the network of urgent care practices include their role in a COVID-19 outbreak and as a part of the solution to the State Government’s hospital demand management strategy.
